Nexus Innovations Incubator sites launched; research agendas set
Testing new models of care and training is key to the transformation of health care through interprofessional practice and education. To that end, eight “pioneer” Nexus Innovations Incubator teams have stepped up to become applied research laboratories for the National Center. The development of the incubator network and the national database is a shared resource model. The National Center provides seed funding and a team of experts, working with each site to leverage and identify their own resources. The goal of the partnership is long-term sustainability of IPE implementation.
 National Center selected the Nexus Innovations Incubator sites based on their already-proven commitment to implementing large-scale interprofessional practice and education initiatives. These programs have considerable experience implementing interprofessional, and they understand the complex issues. This pioneer group will help National Center define its framework for research and evaluation.
National Center selected the Nexus Innovations Incubator sites based on their already-proven commitment to implementing large-scale interprofessional practice and education initiatives. These programs have considerable experience implementing interprofessional, and they understand the complex issues. This pioneer group will help National Center define its framework for research and evaluation.
The incubator members met in September In Minneapolis to establish their research agendas, align them with the National Center’s core research plans, and to discuss the process of collecting data to demonstrate outcomes in real-world settings.
Motivations for the sites to participate are clear. According to Jean Nagelkerk, RN, Ph.D., Vice Provost for Health at Grand Valley State University in Michigan, “The National Center is setting the research agenda for interprofessional education and collaborative practice to support studies that demonstrate the effect that this approach to health care delivery has on achieving the triple aim. Our goal is to improve the healthcare experience in our community by increasing access, enhancing the quality of care, and decreasing costs. The incubator sites will share programmatic strategies, initiatives and best practices in interprofessional education experiences and collaborative practice.”
The Nexus Innovations Incubator sites are focusing on:
Interprofessional education: approaches for preparing team-ready health professionals
Collaborative practice: models of team-based health-focused practice
The Nexus: the true integration of health professions education and health systems
Health outcomes: the health status of individuals and populations who benefit from interprofessional practice and education
“We chose our project because we have unique access to the variables to demonstrate that team handoff reduces cost and improves the health of stroke patients,” explained Andrea Pfeifle, EdD, PT, director, Center for the Advancement of Interprofessional HealthCare, University of Kentucky. “The data are already being collected, we have a team of people who want to do it, and we have the support of enterprise and academic leadership. Everything is lined up.”
The Nexus Innovations Incubator sites are conducting research to demonstrate the added value of the Nexus of practice and education, bringing the two together to achieve better health and educational outcomes. What the incubators learn will actually form National Center data repository from which aggregate data can be used to supplement data from the individual projects. The goal is to prove that the long-sought value that an interprofessional education approach can make a difference in both learning and health outcomes.
“It really comes down to shared vision and shared values. As an academic medical center aligned with the UPMC integrated finance and delivery system, we have a unique laboratory to test and evaluate new models of interprofessional care,” commented Everette James, JD, MBA, associate vice chancellor for health policy and planning and director of the University of Pittsburgh Health Policy Institute. “Rigorous evaluation of the practice environment will help us ensure that our education and training programs reflect the changing delivery system and the needs of a collaboration-ready healthcare workforce. ”
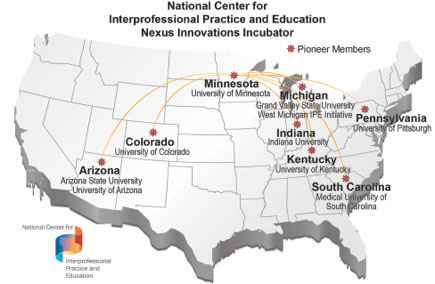
The “pioneer” cohort of higher education and health system partnerships include:
Arizona: To develop a statewide Nexus of practice and education across health systems and multiple educational institutions
Colorado: To demonstrate the value added of students and residents for improving the quality of care during transitions and handoffs
Indiana: Within a healthcare home clinic environment, to engage interprofessional teams of students as navigators for patients at high risk of readmission
Kentucky: To improve the experience and clinical outcomes of stroke patients, particularly across transitions from acute care, to acute rehabilitation, and the community
Michigan: To examine whether the placement of inteprofessional teams of students in a community clinic can increase access to care and improve outcomes of patients with diabetes, and improve staff and patient satisfaction
Minnesota: To transform the model of care through the use of nurses and medical assistants in behaviorial health at family practice clinics, and to explore how the implementation of a new interprofessional student team model can affect outcomes in pediatrics in a Federally Qualified Health Center.
Pennsylvania: To evaluate clinical sites that are developing new care models using advance practice providers ot the full extent of their education and training.
South Carolina: To determine how team-based training and eduation can best meet the needs of clinical sites, including multiple interventions under one umbrella.

Start the Conversation
Every registered user can comment on website content.
Please login or register to comment